Exploring the Connection between Migraine and Hypertension: Are Migraine Patients at Increased Risk of Developing Hypertension?
Migraine and hypertension are two common health conditions that affect millions of people worldwide. While they may seem unrelated, recent research suggests a potential connection between the two. This article delves into the topic of whether migraine patients are at an increased risk of developing hypertension, examining the current scientific evidence and shedding light on the possible mechanisms behind this association.
Understanding Migraine and Hypertension
Migraine: Migraine is a neurological disorder characterized by recurrent episodes of moderate to severe headaches, often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound. It affects approximately 15% of the global population and has a higher prevalence among women.
Hypertension: Hypertension, or high blood pressure, is a chronic condition where the force of blood against the walls of the arteries is consistently too high. It is a significant risk factor for cardiovascular diseases and affects around 1 in 3 adults worldwide.
Population-based studies:
Several population-based studies have investigated the relationship between migraine and hypertension. Some studies suggest that individuals with migraine have a higher prevalence of hypertension compared to those without migraines.A large-scale study published in the American Journal of Medicine in 2020 examined data from over 375,000 individuals and found that migraine patients had a 49% increased risk of developing hypertension compared to non-migraine individuals.
However, it is essential to note that not all studies have consistently shown this association. Some studies have reported conflicting results or found no significant relationship between migraine and hypertension.
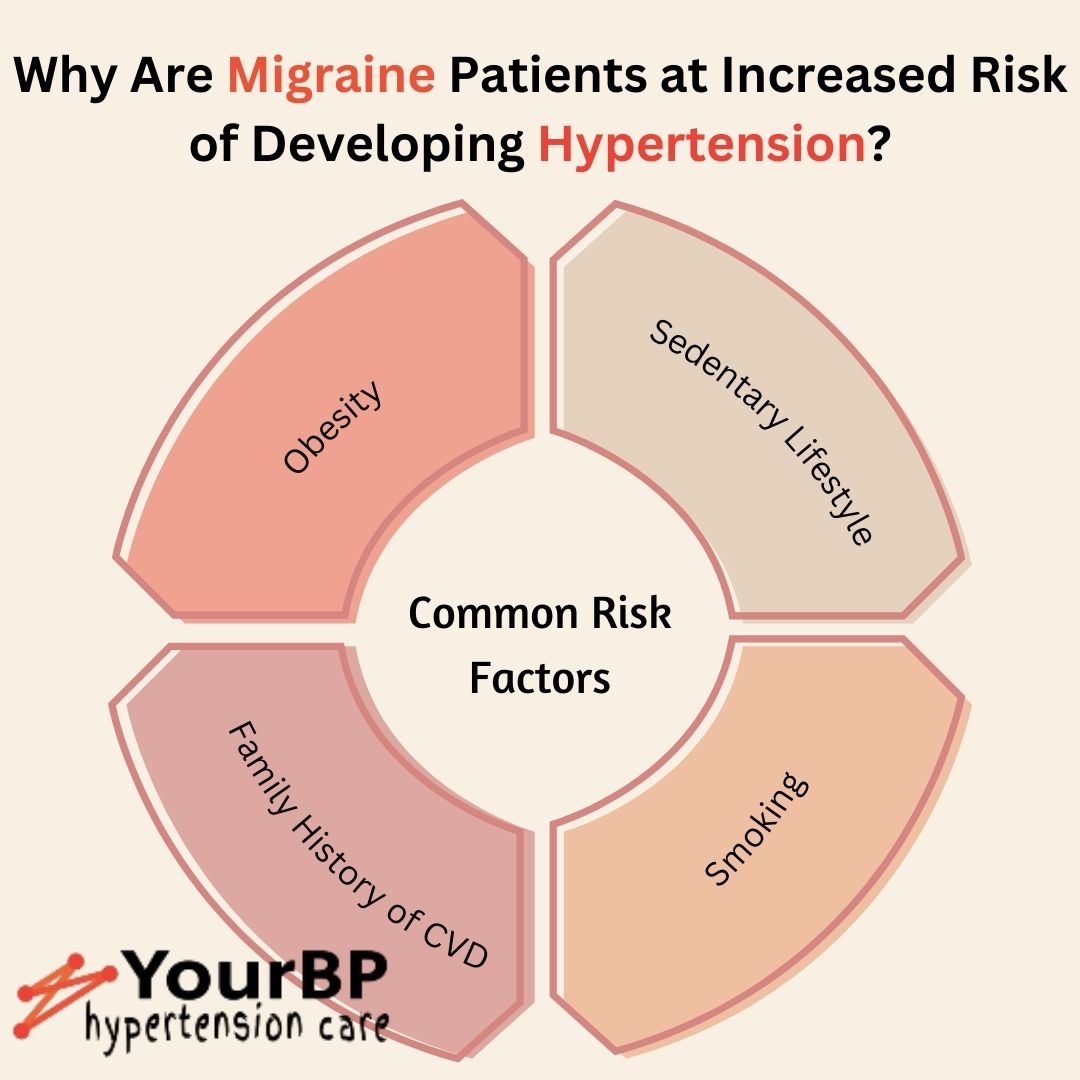
Shared risk factors:
Migraine and hypertension share common risk factors such as obesity, sedentary lifestyle, and family history of cardiovascular diseases. These shared risk factors may contribute to the observed association between the two conditions.A study published in Neurology in 2021 found that individuals with both migraine and hypertension had a higher prevalence of obesity, smoking, and depression compared to those with only one of the conditions.
Possible Mechanisms
Dysregulation of the autonomic nervous system:
Both migraine and hypertension involve dysregulation of the autonomic nervous system, which plays a crucial role in regulating blood pressure. Dysfunction in this system may contribute to the development of both conditions. Research suggests that an overactive sympathetic nervous system and impaired parasympathetic function may be common underlying factors in migraine and hypertension.Endothelial dysfunction and inflammation:
Endothelial dysfunction, characterized by impaired blood vessel function, and chronic inflammation are believed to play a role in both migraine and hypertension.Inflammation and endothelial dysfunction can lead to increased arterial stiffness, reduced nitric oxide availability, and altered blood flow regulation, potentially contributing to the development of both conditions.
Genetic factors:
Genetic predisposition may also contribute to the observed association between migraine and hypertension. Certain genes involved in regulating blood pressure and vascular function have been implicated in both conditions, suggesting a shared genetic basis.Clinical Implications
Improved screening and monitoring:
Considering the potential link between migraine and hypertension, healthcare professionals should be vigilant in screening migraine patients for hypertension and vice versa. Regular blood pressure monitoring and early detection can help prevent the progression of both conditions and reduce the risk of cardiovascular complications.Lifestyle modifications:
Lifestyle modifications, such as maintaining a healthy weight, adopting a balanced diet, regular exercise, stress management, and adequate sleep, are crucial for both migraine and hypertension management. Implementing these lifestyle changes can help reduce the risk of developing hypertension and minimize the frequency and severity of migraines.Conclusion
While the association between migraine and hypertension is still an area of active research, evidence suggests that migraine patients may indeed have an increased risk of developing hypertension. Shared risk factors and underlying mechanisms involving the autonomic nervous system, endothelial dysfunction, inflammation, and genetic factors contribute to this relationship. Understanding this association can help healthcare professionals improve screening and management strategies for patients with both conditions, ultimately promoting better health outcomes.Reference: pubmed.ncbi.nlm.nih.gov, ajmc, ahajournals
Manage your hypertension with YourBP's first of it's kind -- self-care app.
Get it on your Phone
In this Article
- Understanding Migraine and Hypertension
- Examining the Evidence
- Possible Mechanisms
- Clinical Implications
- Conclusion
Also Read
- Hypertension and It's Impact on Lung Health
- Hypertension: Long-Term Consequences and Symptoms
- Natural Ways to Lower High Blood Pressure: Exercise, Yoga, and a Healthy Diet
- Safer Birth Control Methods for People with High Blood Pressure & Cholesterol
- Unveiling the Hidden Clues: Kidney Disease, Hypertension, and Urine Proteins Link
